Animal Disease Models
We specialize in using gene KO mice and pharmacoinhibitors to study the role of chemoattractants and receptors in rodent disease models.
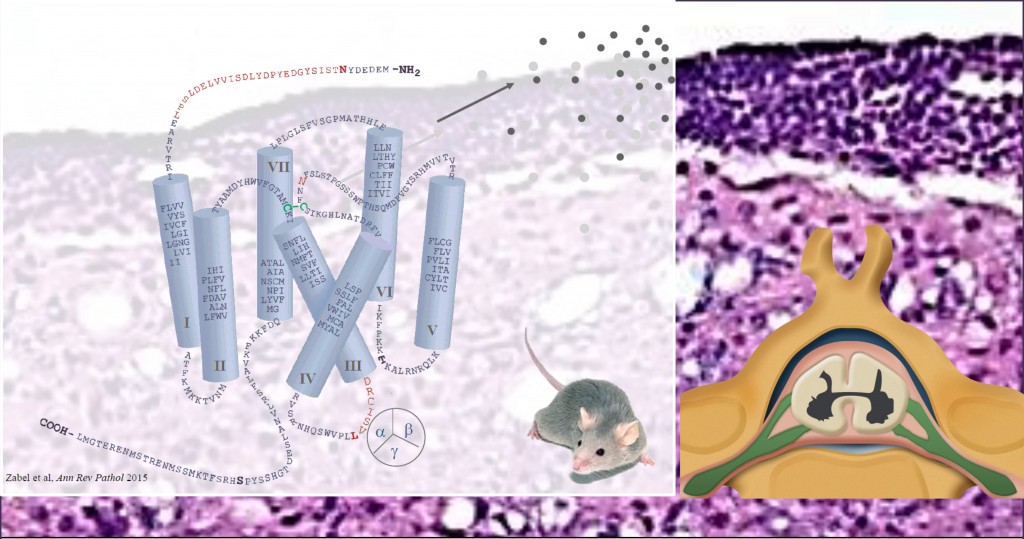
Autoimmune: Experimental Autoimmune Encephalomyelitis. Multiple sclerosis (MS) is a demyelinating disease of the central nervous system (CNS) that affects approximately two million people worldwide. Experimental autoimmune encephalomyelitis (EAE) is a widely studied animal model that shares many clinical and histological features with human MS. Tissue injury in EAE and MS is mediated in part by inflammatory leukocytes that transmigrate across the blood-brain barrier. Therapies that target leukocyte trafficking pathways can reduce disease activity and improve clinical outcomes in MS. Agents that selectively target the trafficking of key inflammatory cell subsets involved in the pathophysiology of MS may therefore be superior to current treatment strategies. We recently showed that CMKLR1-knockout (KO) mice develop less severe clinical and histological EAE than wild-type (WT) mice. CMKLR1 may therefore represent a novel target for the treatment of MS.
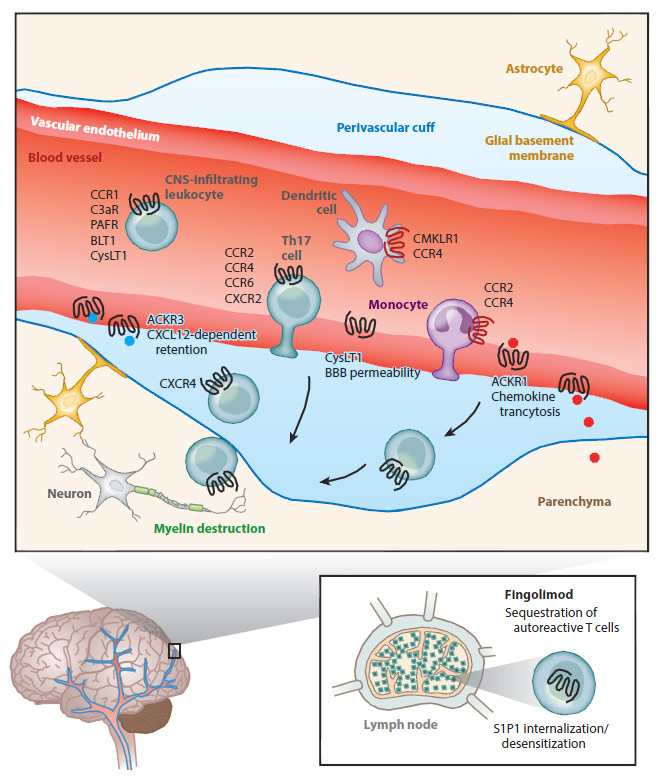
Chemoattractant receptors in the pathogenesis of demyelinating disease. In normal conditions, the blood-brain barrier (BBB) restricts leukocyte access to the central nervous system (CNS). During CNS inflammation, ACKR1 is upregulated on microvascular endothelium and transcytoses chemokines to the lumen to trigger leukocyte recruitment. Chemerin is upregulated in the CNS in experimental autoimmune encephalomyelitis (EAE) mice and can recruit pathogenic CMKLR1+ leukocytes (e.g., dendritic cells). CCR4 also plays a role in dendritic cell recruitment in EAE. The levels of leukotriene B4 (LTB4) and cysteinyl leukotriene (CysLT) are increased in the CNS in EAE mice, leading to increased leukocyte infiltration. CysLT also binds to CysLT receptor 1 (CysLT1) on the microvascular endothelium to increase BBB permeability. CCR2, CCR4, CCR6, and CXCR2 play discrete roles in T helper 17 (Th17) cell recruitment to the CNS, as individual receptor knockout mice are protected against EAE. CCR2 and CCR4 also play roles in monocyte recruitment. Deficiencies in CCR1, C3aR, and platelet-activating factor receptor (PAFR) are also protective in EAE and are associated with reduced leukocyte accumulation in the CNS. Infiltrating leukocytes cross the endothelial barrier and accumulate in perivascular cuffs, where they are normally retained by CXCR4/CXCL12-dependent anchoring. However, during EAE, ACKR3 is upregulated on the endothelium, which leads to increased sequestration of CXCL12, loss of the retention signal, and release of leukocytes to migrate into the parenchyma and target myelin for destruction. (Inset) Fingolimod blocks autoreactive T cell egress from lymph nodes by agonizing sphingosine 1-phosphate receptor 1 (S1P1), resulting in the logjamming of lymphocytes subjacent to cortical sinuses. Zabel et al. Ann Rev Pathol 2015.
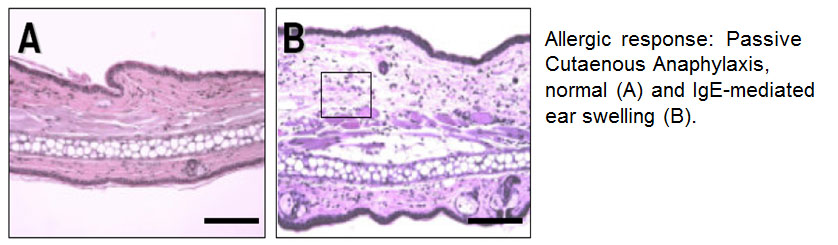
Allergy: Passive Cuatenous Anaphylaxis, Peanut-Induced Anaphylaxis. Using CCRL2 KO mice, we found that the receptor is required for maximal ear swelling and leukocyte infiltration in passive cutaneous anaphylaxis (PCA), a mast cell-dependent in vivo allergy model. Specifically, using mast cell-deficient animals engrafted with either WT or CCRL2 KO bone marrow-cultured mast cells, we show that mast cell-expressed CCRL2 is required for optimal induction of PCA in mice sensitized with a low dose of antigen-specific IgE (high levels of sensitizing antigen abrogated this difference). Thus we conclude that CCRL2 plays a role in modulating in vivo immune responses.
Food allergy affects 6-8% of children under 4 and ~2% of adults in the U.S., and is the number one cause of life-threatening anaphylactic reactions treated in hospital emergency departments. While acute anaphylaxis can be treated with epinephrine, anti-histamines, and steroids, there are currently no proven effective treatments (immunotherapy or otherwise) for food allergy. We hypothesize that CCRL2 plays a pathogenic role in experimental peanut-induced anaphylaxis (PIA).
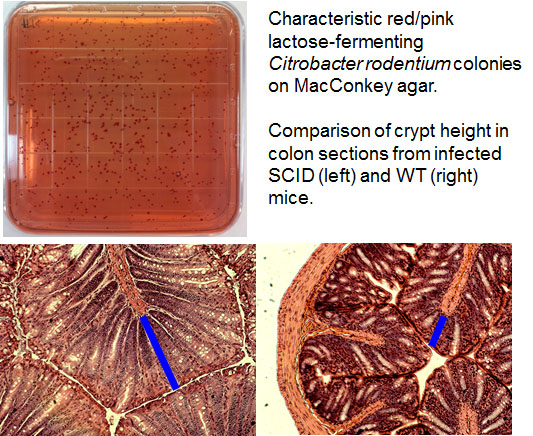
Infectious: Citrobacter rodentium-induced Colitis. C. rodentium is an attaching and effacing bacterial pathogen that colonizes the intestinal epithelium of mice, leading to colitis and colonic hyperplasia. It serves as a model for the human bacterial pathogens enteropathogenic E. coli (EPEC) and enterohemorrhagic E. coli (EHEC), which are responsible for severe food poisoning worldwide, and may contribute to chronic gastrointestinal inflammatory bowel diseases such as Crohn’s disease. All three pathogens intimately adhere to the gut epithelium and cause brush border effacement, which ultimately leads to pathologic alterations in the colon.
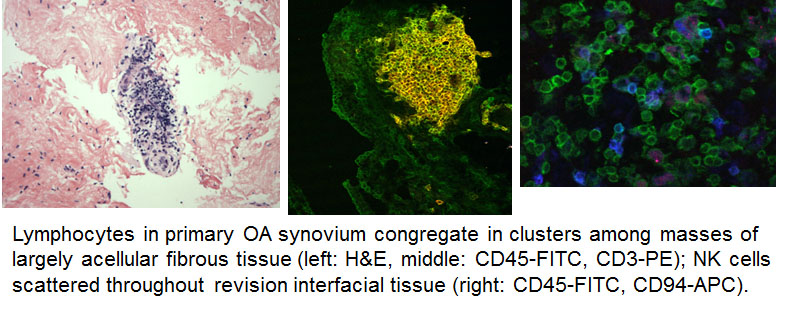
Inflammatory Disorders: Osteoarthritis and Peri-Prosthetic Inflammation. Patients with degenerative joint disease (most commonly OA) that is refractory to conservative management are candidates for TJR, which alleviates pain and restores limb function in >80% of cases. Aseptic loosening of joint prostheses is the most significant long-term complication, occurring in 7-18% of patients at 25-year follow up, and requires many to undergo revision surgery. The loss of bony fixation is due to inflammatory responses triggered by wear particles generated at the bearing surfaces and along the implant interface. We recently showed 1) NK cells are a principal synovial tissue infiltrating lymphocyte subset in patients with OA and particle-mediated peri-prosthetic inflammation; 2) the infiltrating tissue NK cells are functionally distinct from blood NK cells, and respond poorly to stimulation as measured by IFN- production; 3) SF from the patients contains NK cell chemoattractants (including chemerin) and NK cell-activating cytokines; and 4) synovial tissue NK cells express CCR5 and CXCR3.
Cancer: CXCR7+ Leukemias.